Is your case great enough to be selected for our Wall of Fame? If so, we’ll post your name and case here for the world to see!
10/23: Evgenii Chernov
Best Disease
9/24: Anjana Mirajkar and Manish Nagpal
Intraocular Foreign Body
8/24: Anjana Mirajkar and Manish Nagpal
Pseudopapilledema from leukemic optic nerve infiltration
7/24: Justin Grassmeyer, Ambar Faridi, and Brittany Heckerman
Lattice degeneration
6/24: Ogugua Okonkwo, Adekunle Olubola Hassan, Ayodele Harriman, Ogochukwu Sibeudu, and Idris Akintayo Oyekunle
Tuberculous serpiginous-like choroiditis
5/24: Seif Anwar
Inherited Retinal Disease
Sengül Özdek and Ece Özdemir Zeydanlı
Case of the Year winner!
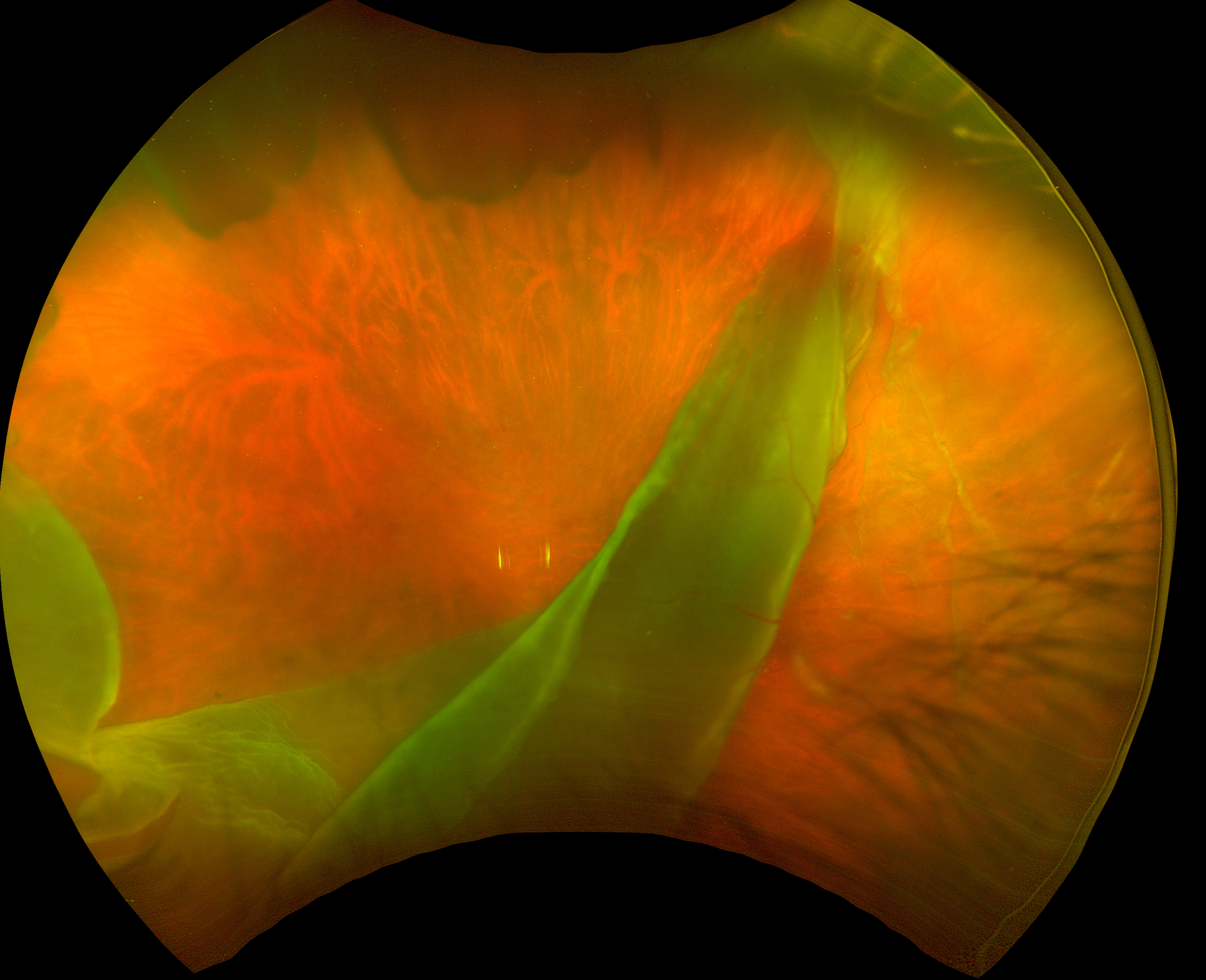
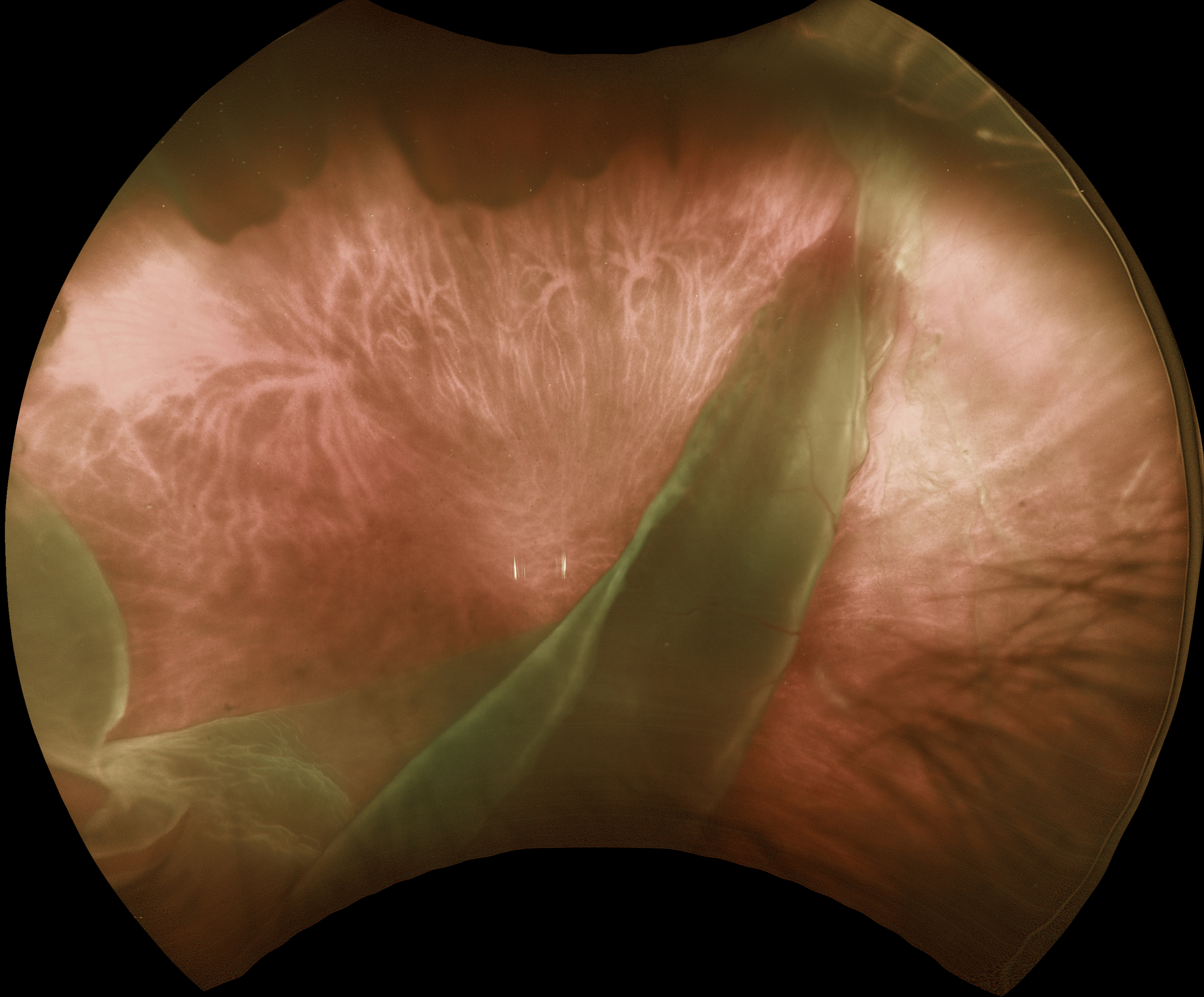
Retinal Arteriovenous Malformation
4/24: Kanwaljeet Harjot Madan
Shaken baby syndrome
3/24: Ayushi Gupta and Vishal Agrawal
Benign familial fleck retina
2/24: Will Gibson
Retinal venous malformation
12/23: Anjana Mirajkar and Manish Nagpal
Central retinal artery occlusion with cilioretinal sparing
11/23: Anjana Mirajkar and Manish Nagpal
Harada’s Disease
10/23: Will Gibson
Posterior scleritis with chorioretinal folds
9/23: Shivraj Tagare and Nishant Maindargi
Valsalva retinopathy drained with YAG laser
8/23: Mohammad Abbas
Laser-induced retinal break and vitreous hemorrhage
7/23: Joe Yuenpang Cheung
Group-type congenital pigmented nevi of the RPE (bear tracks)
6/23: Gil Calvão-Santos and Keissy Sousa
Waardenburg Syndrome
5/23: Natasa Draca and Ratko Lazic
Tattoo-induced Uveitis
4/23: Veronika Matello and Barbara Parolini
Case of the Year winner!
The EmPuzzled Eye
3/23: Emma Oreskovic and Natasha Draca
Optic Nerve Pit
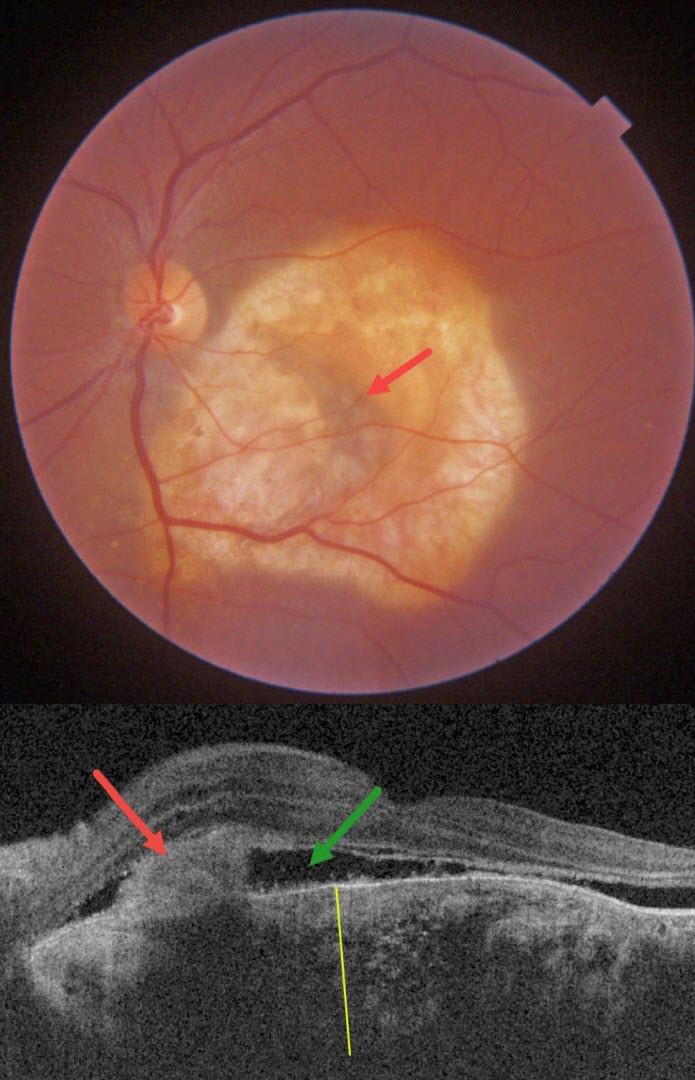
2/23: Anjana Mirajkar
Giant RPE Tear
11/22: Veronika Matello and Barbara Parolini
Choroidal Hemangioma Widefield OCT
8/22: Nivesh Gupta
Ischemic Central Retinal Vein Occlusion
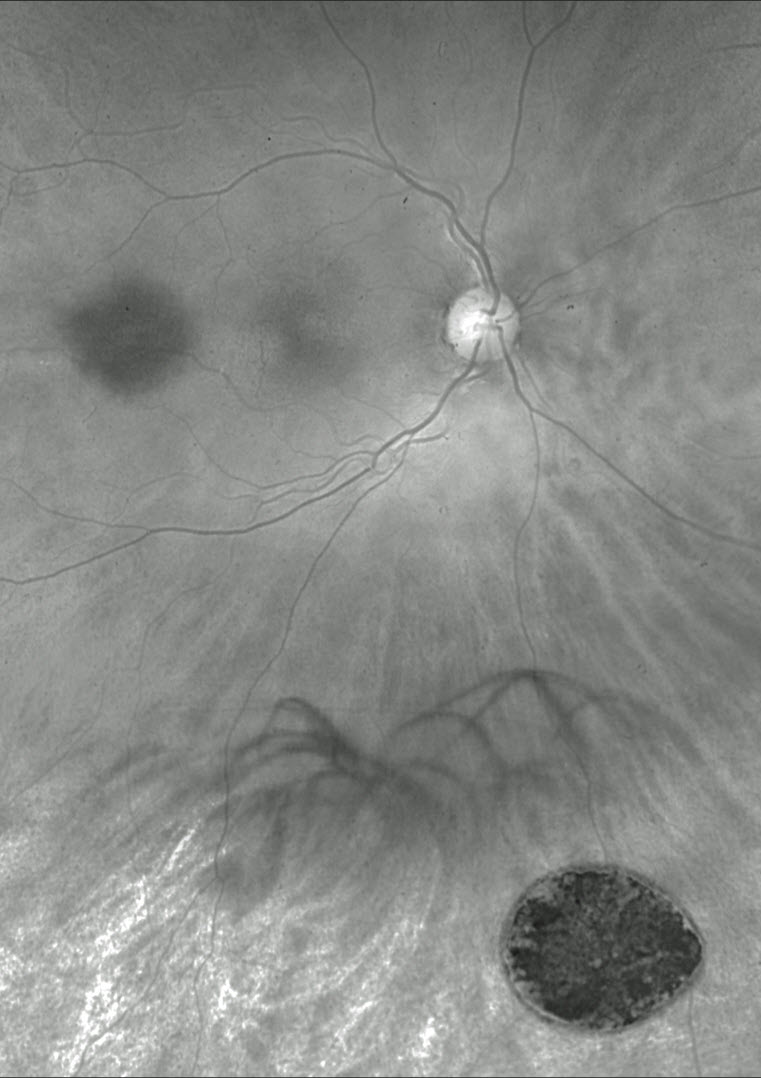
7/22: Omar Mulki:
Choroidal Osteoma
3/22: Erdem Dinç
Is Temporary ILM Flap Sufficient for MH Closure?
1/22: Veronika Matello and Barbara Parolini
Case of the Year winner!
Choroidal Transplant for Subfoveal AMD MNV
12/21: Otis Hertsenberg
Optic Nerve Coloboma with Pit
11/21: David Kilpatrick
Frosted Branch Angiitis from Sarcoidosis
10/21: Kumar Chugani
Coats Disease